Although cardiac arrhythmias can be treated successfully even in the newborn period, arrhythmias can also arise as a result of surgical repair. An advanced cardiac mapping system in place at St. Louis Children’s Hospital has proven to be a valuable tool in recognizing the origins of arrhythmias and presenting a range of therapeutic options.
Although cardiac arrhythmias can be treated successfully even in the newborn period, arrhythmias can also arise as a result of surgical repair. An advanced cardiac mapping system in place at St. Louis Children’s Hospital has proven to be a valuable tool in recognizing the origins of arrhythmias and presenting a range of therapeutic options.
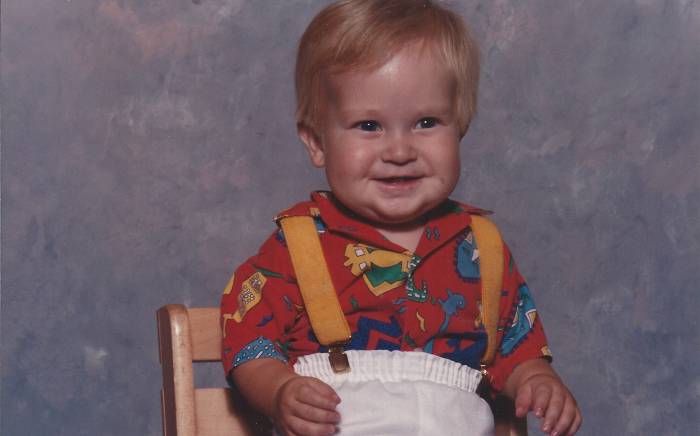
At 8 months old, Correy Nehring was diagnosed at St. Louis Children’s Hospital with complex congenital heart disease consisting of a hypoplastic right ventricle with tricuspid atresia. Because Correy had no blood flow from the right atrium to the right ventricle, her doctors at St. Louis Children's Hospital, created a Glenn shunt to improve her oxygen saturation and decrease the volume load on the single ventricle. At age 3, Correy required a modified Fontan procedure, and eventually her right ventricle began to grow and function almost normally. Two years later, she was able to have her Fontan reversed.
Although Correy entered kindergarten with no evidence of symptoms, a profoundly slow heart rate was found and required a pacemaker. Now in her senior year of high school, and under the care of Mark Johnson, MD, Attending Physician in the cardiology division and WUSM Associate Professor of Pediatrics, Correy developed a new problem: episodes of sudden rapid heart rate. This presented yet another challenge to the cardiology team.
Dr. Johnson consulted electrophysiologists George Van Hare, MD, and Jennifer Silva, MD, to examine Correy. They found that abnormal electrical connections in her heart due to her congenital heart anomalies, as well as the surgery that had been done, were causing her rapid heart rate episodes. "Correy’s care is a group effort and a great example of how we all work as a team to care for kids," says Dr. Silva, who serves as director of the Electrophysiology Lab (EP) and WUSM Instructor in Pediatrics. "After medication management failed to correct her abnormal rhythms, Dr. Van Hare and I concluded that a transcatheter ablation was the best strategy for Correy."
While inside Correy’s heart, these specialists created a three-dimensional electrical map to first find the cause of Correy’s abnormal rhythm. "The mapping tool helped to clearly define the edges of her scar so we could successfully ablate each area," describes Dr. Silva. "Correy presented us a highly complex case, and we identified three different substrates of arrhythmia."
According to Dr. Van Hare, director of the Division of Pediatric Cardiology at Washington University School of Medicine and the Louis Larrick Ward Chair in Pediatric Cardiology at St. Louis Children's Hospital, a pediatric electrophysiology program is defined by its ability to take on and treat cases like Correy’s arrhythmia. "She, like hundreds of other children with arrhythmia conditions who have come to St. Louis Children’s Hospital, requires not only the most sophisticated tools available, but also an experienced team accustomed to volume and complexity," says Dr. Van Hare.
For the past three years, the EP Lab at St. Louis Children’s Hospital has used sophisticated 3D cardiac mapping in the treatment of pediatric cardiac arrhythmias. Not only does this 3D technology facilitate various treatment modalities, real-time navigation of the heart provides greater procedure success and reduced radiation exposure for patients.
A series of patches are placed on the patient’s chest, which allows a highly sophisticated computer to calculate where the tip of the catheter is located in 3D space at all times. By moving the catheter through the heart, specialists can construct a 3D model on a computer screen of the inner surface of the heart, from the valves to the veins that come into the heart. "At the same time, we can record the electrical signals from everywhere we touch in the heart," reports Dr. Van Hare. "This information tells us where important structures are located, such as scars, valves and patches from prior surgery. We also use it to map the course of electrical activation as it moves through the heart during normal and abnormal rhythms. Doing all this together allows us to understand what is actually supporting and causing these abnormal heart rhythms, and then to select the best location in the heart for ablation."
 According to Dr. Silva, an additional benefit of cardiac mapping especially important to children is the reduced need for fluoroscopy. "Once the map is developed, we no longer require X-ray," she adds. "For patients like Correy facing a six-hour procedure, this is a significant reduction in radiation exposure for our patients."
According to Dr. Silva, an additional benefit of cardiac mapping especially important to children is the reduced need for fluoroscopy. "Once the map is developed, we no longer require X-ray," she adds. "For patients like Correy facing a six-hour procedure, this is a significant reduction in radiation exposure for our patients."
In addition to cardiac mapping, Dr. Silva’s fellowship training was devoted to research into understanding the prime location to pace a heart to achieve maximum contraction. Her first three years of training were completed at St. Louis Children’s Hospital, with the fourth year at Boston Children’s Hospital. She returned this past fall to lead the EP program and continue her research. Mark Levin, MD, recently joined the department from Children’s Hospital in Philadelphia. Dr. Levin, WUSM Instructor in Pediatrics, is a pediatric cardiologist and a basic science researcher focused on understanding cellular electrophysiology.
"Here, we have highly experienced physicians who work well as a team, and while they’re taking care of patients, these clinicians are also thinking about how to advance the field on all fronts," shares Dr. Van Hare, who came to Washington University and St. Louis Children’s Hospital 18 months ago from Stanford University.
"Having a free-standing children’s hospital attached to an adult hospital is the ideal scenario," he says. "Not every hospital has a catheterization laboratory with a pediatric orientation and access to adult expertise if needed. Today, we have a very different- looking team, which is a major advance for patients. Because of our strong cardiac program with committed pediatric cardiac anesthesia, nurses and technicians, we are accustomed to caring for a high volume of very sick children."
In treating cardiac arrhythmias, there are patients for whom medication is the right answer. Ablation techniques offer patients an opportunity for cure with few complications with a low recurrence rate. Some cases call for implantable devices, including basic pacemakers that pace one segment of the heart, cardiac resynchronization therapy (CRT) pacemakers that attempt to improve total synchronization functionality, and finally implantable cardioverter-defibrillators (ICDs), which protect against life-threatening arrhythmias.
"Because of our large heart failure population, it’s a natural fit for us to take a close look at CRT to find ways to select the patients who will benefit most from these devices," Dr. Van Hare remarks. "For a good number of our patients, we’ve at least been able to delay the need for heart transplantation so that they can become healthier and stronger. The best outcome we can possibly expect is to dodge a heart transplant completely."